What Causes Feet To Over Pronate
The majority of the population have a normal to low arch. Even though the arches appear to be normal most of us suffer from over-pronation during walking, running and standing, due to the hard, flat unnatural surfaces we walk on, combined with wearing unsupportive footwear. With every step we take the arches flatten and the ankles roll inwards. Pronation itself is not wrong because we need to pronate and supinate as part of our natural gait cycle. Pronation (rolling in) acts as a shock-absorbing mechanism and supination (rolling out) helps to propel our feet forward. Over-pronation occurs when the foot pronates too deep and for too long, not allowing the foot to 'recover' and supinate. Over-pronation hampers our natural walking pattern. It causes an imbalance and leads to wear and tear in several parts of the body with every step we take.

Causes
Over-pronation occurs when the foot collapses too far inward stressing the plantar fascia (the area underneath the arch of the foot.) Normally, one pronates every time he or she walks, but excessive pronation is called over-pronation. When this occurs it can cause pain in the feet, knees, hips, low back and even the shoulder. Decreasing over-pronation, which is very prominent in runners, will help add endurance, speed and efficiency to your run and ultimately place less stress on your body.
Symptoms
When standing, your heels lean inward. When standing, one or both of your knee caps turn inward. Conditions such as a flat feet or bunions may occur. You develop knee pain when you are active or involved in athletics. The knee pain slowly goes away when you rest. You abnormally wear out the soles and heels of your shoes very quickly.
Diagnosis
People who overpronate have flat feet or collapsed arches. You can tell whether you overpronate by wetting your feet and standing on a dry, flat surface. If your footprint looks complete, you probably overpronate. Another way to determine whether you have this condition is to simply look at your feet when you stand. If there is no arch on the innermost part of your sole, and it touches the floor, you likely overpronate. The only way to truly know for sure, however, is to be properly diagnosed by a foot and ankle specialist.

Non Surgical Treatment
Mild cases of Overpronation may be controlled or corrected with a supportive shoe that offers medial support to the foot along with a strong heel counter to control excessive motion at the heel starting with heel strike. In mild cases with no abnormal mechanical pressures, an over the counter orthotic with heel cup and longitudinal or medial arch support to keep the foot from progressing past neutral may help to realign the foot. A Custom foot orthotic with heel cup and longitudinal arch support to help correct position of the foot as it moves through motion. Heel wedges may also assist in correcting motion.
Surgical Treatment
Calcaneal "Slide" (Sliding Calcaneal Osteotomy) A wedge is cut into the heel bone (calcaneus) and a fixation device (screws, plate) is used to hold the bone in its new position. This is an aggressive option with a prolonged period of non-weightbearing, long recovery times and many potential complications. However, it can and has provided for successful patient outcomes.
The Way To Spot Severs Disease?
Sever's disease, or calcaneal apophysitis, is a common cause of heel pain among active children between 10 to 13 years old. This spontaneous heel pain results from injury to the heel bone?s growth plate which is caused by overuse rather than specific injury or trauma. The condition is common among athletic children, particularly those active in soccer, football, and baseball. Treatment is available to reduce pain and discomfort associated with Sever's disease, but the condition usually resolves on its own once feet stop growing.
Causes
Your child is most at risk for this condition when he or she is in the early part of the growth spurt in early puberty. Sever's disease is most common in physically active girls 8 years to 10 years of age and in physically active boys 10 years to 12 years of age. Soccer players and gymnasts often get Sever's disease, but children who do any running or jumping activity may also be at an increased risk. Sever's disease rarely occurs in older teenagers because the back of the heel has typically finished growing by 15 years of age.
Symptoms
Pain is usually related to activity levels. In most cases the posterior aspect of the calcaneus will be tender. Checking both the medial and lateral aspects of the posterior portion of the growth plate will often show tenderness. Occasionally, the plantar aspect may be tender or both of these locations may be found to be tender. Frequently the Achilles tendon is tight and there may have been a recent increase in activity. The factors contributing to this disorder are similar to those causing plantar fasciitis, but a tight Achilles tendon appears to be a greater contributor than pronation.
Diagnosis
Sever disease is most often diagnosed clinically, and radiographic evaluation is believed to be unnecessary by many physicians, but if a diagnosis of calcaneal apophysitis is made without obtaining radiographs, a lesion requiring more aggressive treatment could be missed. Foot radiographs are usually normal and the radiologic identification of calcaneal apophysitis without the absence of clinical information was not reliable.
Non Surgical Treatment
Orthotics, The orthotics prescribed are made to align the foot in its correct foot posture. This will reduce stress and force at the site of the growth plate of the heel bone. Rest and Ice the heel 20 minutes before and after sporting activity. Calf muscle stretching exercises.
Prevention
Perform a well rounded dynamic warm up before activity. Perform a good static stretching routine after activity. Increase core strength. Perform exercises that emphasize active lengthening of the calf muscles. Use proper footwear. Avoid excessive running or jumping on hard surfaces like concrete by using better surfaces such as asphalt, gymnasium floors or grass.
Acquired Flat Foot Deformity Surgery
Overview
This condition is a progressive collapse of the tendons and ligaments that hold up the foot?s arch. This condition most commonly affects women. It typically occurs in only one foot, but in some cases, both feet are afflicted. 
Causes
There are multiple factors contributing to the development of this problem. Damage to the nerves, ligaments, and/or tendons of the foot can cause subluxation (partial dislocation) of the subtalar or talonavicular joints. Bone fracture is a possible cause. The resulting joint deformity from any of these problems can lead to adult-acquired flatfoot deformity. Dysfunction of the posterior tibial tendon has always been linked with adult-acquired flatfoot deformity (AAFD). The loss of active and passive pull of the tendon alters the normal biomechanics of the foot and ankle. The reasons for this can be many and varied as well. Diabetes, high blood pressure, and prolonged use of steroids are some of the more common causes of adult-acquired flatfoot deformity (AAFD) brought on by impairment of the posterior tibialis tendon. Overstretching or rupture of the tendon results in tendon and muscle imbalance in the foot leading to adult-acquired flatfoot deformity (AAFD). Rheumatoid arthritis is one of the more common causes. About half of all adults with this type of arthritis will develop adult flatfoot deformity over time. In such cases, the condition is gradual and progressive. Obesity has been linked with this condition. Loss of blood supply for any reason in the area of the posterior tibialis tendon is another factor. Other possible causes include bone fracture or dislocation, a torn or stretched tendon, or a neurologic condition causing weakness.
Symptoms
Not everyone with adult flatfoot has problems with pain. Those who do usually experience it around the ankle or in the heel. The pain is usually worse with activity, like walking or standing for extended periods. Sometimes, if the condition develops from arthritis in the foot, bony spurs along the top and side of the foot develop and make wearing shoes more painful. Diabetic patients need to watch for swelling or large lumps in the feet, as they may not notice any pain. They are also at higher risk for developing significant deformities from their flatfoot.
Diagnosis
The adult acquired flatfoot, secondary to posterior tibial tendon dysfunction, is diagnosed in a number of ways with no single test proven to be totally reliable. The most accurate diagnosis is made by a skilled clinician utilizing observation and hands on evaluation of the foot and ankle. Observation of the foot in a walking examination is most reliable. The affected foot appears more pronated and deformed compared to the unaffected foot. Muscle testing will show a strength deficit. An easy test to perform in the office is the single foot raise. A patient is asked to step with full body weight on the symptomatic foot, keeping the unaffected foot off the ground. The patient is then instructed to "raise up on the tip toes" of the affected foot. If the posterior tibial tendon has been attenuated or ruptured, the patient will be unable to lift the heel off the floor and rise onto the toes. In less severe cases, the patient will be able to rise on the toes, but the heel will not be noted to invert as it normally does when we rise onto the toes. X-rays can be helpful but are not diagnostic of the adult acquired flatfoot. Both feet - the symptomatic and asymptomatic - will demonstrate a flatfoot deformity on x-ray. Careful observation may show a greater severity of deformity on the affected side.
Non surgical Treatment
Treatment depends very much upon a patient?s symptoms, functional goals, degree and specifics of deformity, and the presence of arthritis. Some patients get better without surgery. Rest and immobilization, orthotics, braces and physical therapy all may be appropriate. With early-stage disease that involves pain along the tendon, immobilization with a boot for a period of time can relieve stress on the tendon and reduce the inflammation and pain. Once these symptoms have resolved, patients are often transitioned into an orthotic that supports the inside aspect of the hindfoot. For patients with more significant deformity, a larger ankle brace may be necessary. 
Surgical Treatment
For those patients with PTTD that have severe deformity or have not improved with conservative treatments, surgery may be necessary to return them to daily activity. Surgery for PTTD may include repair of the diseased tendon and possible tendon transfer to a nearby healthy tendon, surgery on the surrounding bones or joints to prevent biomechanical abnormalities that may be a contributing factor or both.
Adult Aquired FlatFoot
There are some things that gain value as they age. Antique dealers are always on the lookout for pieces that have a certain wear and tear look that will bring a high price tag. Our feet on the other hand, don't always fair as well when they have experienced a lot of wear and tear. Cumulative stress and impact can cause your foot structure to weaken and become prone to injury, especially when you have a flat foot. This is the case with a condition called posterior tibial tendon dysfunction.

Causes
Flat feet causes greater pressure on the posterior tibial tendon than normal. As the person with flat feet ages, the muscles, tendons and ligaments weaken. Blood supplies diminish as arteries narrow. These conditions are magnified for obese patients because of their increased weight and atherosclerosis. Finally, the tendon gives out or tears. Most of the time, this is a slow process. Once the posterior tibial tendon and ligaments stretch, body weight causes the bones of the arch to move out of position. The foot rotates inward (pronation), the heel bone is tilted to the inside, and the arch appears collapsed. In some cases, the deformity progresses until the foot dislocates outward from the ankle joint.
Symptoms
Often, this condition is only present in one foot, but it can affect both. Adult acquired flatfoot symptoms vary, but can swelling of the foot's inner side and aching heel and arch pain. Some patients experience no pain, but others may experience severe pain. Symptoms may increase during long periods of standing, resulting in fatigue. Symptoms may change over time as the condition worsens. The pain may move to the foot's outer side, and some patients may develop arthritis in the ankle and foot.
Diagnosis
Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility.
Non surgical Treatment
Medical or nonoperative therapy for posterior tibial tendon dysfunction involves rest, immobilization, nonsteroidal anti-inflammatory medication, physical therapy, orthotics, and bracing. This treatment is especially attractive for patients who are elderly, who place low demands on the tendon, and who may have underlying medical problems that preclude operative intervention. During stage 1 posterior tibial tendon dysfunction, pain, rather than deformity, predominates. Cast immobilization is indicated for acute tenosynovitis of the posterior tibial tendon or for patients whose main presenting feature is chronic pain along the tendon sheath. A well-molded short leg walking cast or removable cast boot should be used for 6-8 weeks. Weight bearing is permitted if the patient is able to ambulate without pain. If improvement is noted, the patient then may be placed in custom full-length semirigid orthotics. The patient may then be referred to physical therapy for stretching of the Achilles tendon and strengthening of the posterior tibial tendon. Steroid injection into the posterior tibial tendon sheath is not recommended due to the possibility of causing a tendon rupture. In stage 2 dysfunction, a painful flexible deformity develops, and more control of hindfoot motion is required. In these cases, a rigid University of California at Berkley (UCBL) orthosis or short articulated ankle-foot orthosis (AFO) is indicated. Once a rigid flatfoot deformity develops, as in stage 3 or 4, bracing is extended above the ankle with a molded AFO, double upright brace, or patellar-tendon-bearing brace. The goals of this treatment are to accommodate the deformity, prevent or slow further collapse, and improve walking ability by transferring load to the proximal leg away from the collapsed medial midfoot and heel.

Surgical Treatment
If surgery is necessary, a number of different procedures may be considered. The specifics of the planned surgery depend upon the stage of the disorder and the patient?s specific goals. Procedures may include ligament and muscle lengthening, removal of the inflamed tendon lining, tendon transfers, cutting and realigning bones, placement of implants to realign the foot and joint fusions. In general, early stage disease may be treated with tendon and ligament (soft-tissue) procedures with the addition of osteotomies to realign the foot. Later stage disease with either a rigidly fixed deformity or with arthritis is often treated with fusion procedures. If you are considering surgery, your doctor will speak with about the specifics of the planned procedure.
What Are The Most Obvious Main Treatments And Causes Of Achilles Tendonitis Painfulness ?
 Achilles tendinitis is an overuse injury common in many sports that require lots of running and jumping. Once this condition becomes more chronic adhesions that form along the tissues and the injury becomes more of a tendinosis. Treatment for a tendinosis is much different that for a tendinitis, so it is important to recognize what stage the injury is at in order to treat it appropriately. An acute achilles tendinitis involves inflammation and would be treated with rest, ice, etc. Once the inflammation has decreased, research shows that eccentric exercises are beneficial. Once there is tendinosis, it becomes imperative to break up those adhesions with ART and prescribe appropriate stretches and exercises.
Achilles tendinitis is an overuse injury common in many sports that require lots of running and jumping. Once this condition becomes more chronic adhesions that form along the tissues and the injury becomes more of a tendinosis. Treatment for a tendinosis is much different that for a tendinitis, so it is important to recognize what stage the injury is at in order to treat it appropriately. An acute achilles tendinitis involves inflammation and would be treated with rest, ice, etc. Once the inflammation has decreased, research shows that eccentric exercises are beneficial. Once there is tendinosis, it becomes imperative to break up those adhesions with ART and prescribe appropriate stretches and exercises.
Causes
Tendinitis can result from an injury or over-use. Improper stretching prior to exertion or incorrect form during physical activity can also contribute to the development of tendinitis. Some people, including those with ?flat feet,? tight tendons or arthritis, are particularly prone to tendinitis.
Symptoms
Patients with an Achilles tendon rupture frequently present with complaints of a sudden snap in the lower calf associated with acute, severe pain. The patient reports feeling like he or she has been shot, kicked, or cut in the back of the leg, which may result in an inability to ambulate further. A patient with Achilles tendon rupture will be unable to stand on his or her toes on the affected side. Tendinosis is often pain free. Typically, the only sign of the condition may be a palpable intratendinous nodule that accompanies the tendon as the ankle is placed through its range of motion (ROM). Patients with paratenonitis typically present with warmth, swelling, and diffuse tenderness localized 2-6 cm proximal to the tendon's insertion. Paratenonitis with tendinosis. This is diagnosed in patients with activity-related pain, as well as swelling of the tendon sheath and tendon nodularity.
Diagnosis
Confirming Achilles tendonitis may involve imaging tests. X-rays provide images of the bones of the foot and leg. Magnetic resonance imaging (MRI) is useful for detecting ruptures and degeneration of tissue. Ultrasound shows tendon movement, related damage, and inflammation.
Nonsurgical Treatment
Physical therapy is the first and most useful defense for achilles tendonitis because of the two presentations outlined above. Treatments for the two types are quite different in approach. Midsubstance tendinitis responds well to stretching, whereas insertional tendnitis tends to be aggravated more by it. Depend on your trusted physical therapist to differentiate between the two and follow their guidelines on exercises and running modifications. Running gait patterns that show excessive ?sinking postures? tend to point to the source of achilles tendon problems. Altering your gait in the midstance phase of the cycle can reduce the load on the tendon dramatically and thereby reduce pain. Rely on your running physical therapist for proper guidance on altering your gait the right way. Stride Strong?s Portland Running Clinic gait analysis can identify and fix potential issues before pain sets in. Icing at the onset of acute achilles pain (i.e. when the injury is fresh and new) would help control the inflammation. Your next step should be to call our number for an appointment.

Surgical Treatment
There are two types of Achilles repair surgery for tendonitis (inflammation of the Achilles Tendon), if nonsurgical treatments aren't effective. Gastrocnemius recession - The orthopaedic surgeon lengthens the calf muscles to reduce stress on your Achilles tendon. D?bridement and repair - During this procedure, the surgeon removes the damaged part of the Achilles tendon and repairs the remaining tendon with sutures or stitches. Debridement is done when the tendon has less than 50% damage.
Prevention
Appropriately warm up and stretch before practice or competition. Allow time for adequate rest and recovery between practices and competition. Maintain appropriate conditioning, Ankle and leg flexibility, Muscle strength and endurance, Cardiovascular fitness. Use proper technique. To help prevent recurrence, taping, protective strapping, or an adhesive bandage may be recommended for several weeks after healing is complete.
What Is Heel Pain

Overview
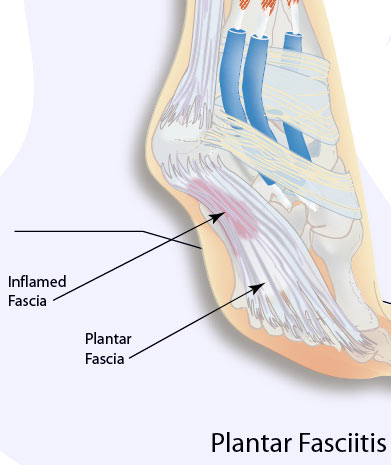
Plantar fasciitis is the pain caused by degenerative irritation at the insertion of the plantar fascia on the medial process of the calcaneal tuberosity. The pain may be substantial, resulting in the alteration of daily activities. Various terms have been used to describe plantar fasciitis, including jogger’s heel, tennis heel, policeman’s heel, and even gonorrheal heel. Although a misnomer, this condition is sometimes referred to as heel spurs by the general public.
Causes
Plantar fasciitis tends to strike those who overtrain, neglect to stretch their calf muscles, or overdo hill work and speedwork. Plantar fasciitis can also be caused by biomechanical flaws, including flat, high-arched feet and a tight Achilles tendon; excessive pronation; sudden increases in training mileage; beginning speedwork; wearing worn running shoes; running on hard surfaces, like asphalt or concrete; or wearing high heels all day before switching into flat running shoes.
Symptoms
Plantar fasciitis and heel spur pain usually begins in the bottom of the heel, and frequently radiates into the arch. At times, however, the pain may be felt only in the arch. The pain is most intense when first standing, after any period of rest. Most people with this problem experience their greatest pain in the morning, with the first few steps after sleeping. After several minutes of walking, the pain usually becomes less intense and may disappear completely, only to return later with prolonged walking or standing. If a nerve is irritated due to the swollen plantar fascia, this pain may radiate into the ankle. In the early stages of Plantar Fasciitis and Heel Spurs, the pain will usually subside quickly with getting off of the foot and resting. As the disease progresses, it may take longer periods of time for the pain to subside.
Diagnosis
A physical exam performed in the office along with the diagnostic studies as an x-ray. An MRI may also be required to rule out a stress fracture, or a tear of the plantar fascia. These are conditions that do not normally respond to common plantar fasciitis treatment.
Non Surgical Treatment
In general, we start by correcting training errors. This usually requires relative rest, the use of ice after activities, and an evaluation of the patient's shoes and activities. Next, we try correction of biomechanical factors with a stretching and strengthening program. If the patient still has no improvement, we consider night splints and orthotics. Finally, all other treatment options are considered. Non-steroidal anti-inflammatory medications are considered throughout the treatment course, although we explain to the patient that this medicine is being used primarily for pain control and not to treat the underlying problem.

Surgical Treatment
Surgery may be considered in very difficult cases. Surgery is usually only advised if your pain has not eased after 12 months despite other treatments. The operation involves separating your plantar fascia from where it connects to the bone; this is called a plantar fascia release. It may also involve removal of a spur on the calcaneum if one is present. Surgery is not always successful. It can cause complications in some people so it should be considered as a last resort. Complications may include infection, increased pain, injury to nearby nerves, or rupture of the plantar fascia.
What Is Heel Pain And The Way To End It
Overview
Plantar Fasciitis is the most common condition of heel pain. This condition occurs when the long fibrous plantar fascia ligament along the bottom of the foot develops tears in the tissue resulting in pain and inflammation. The pain of plantar fasciitis is usually located close to where the fascia attaches to the calcaneous, also known as the heel bone. The condition is often misspelled as: plantar fascitis, plantar fasciatis, planters fasciitis, plantar faciatis, and plantar faciaitis. Plantar fasciitis causes the inflammation of the plantar fascia ligament which runs along the bottom of the foot. The plantar fascia ligament is made of fibrous bands of tissue and runs between the heel bone and your toes and stretches with every step. Inflammation develops when tears occur in the tissue. The most common complaint from plantar fasciitis is a burning, stabbing, or aching pain in the heel of the foot. Most sufferers will be able to feel it in the morning because the fascia ligament tightens up during the night while we sleep, causing pain to diminish. However, when we climb out of bed and place pressure on the ligament, it becomes taut and pain is particularly acute. Pain usually decreases as the tissue warms up, but may easily return again after long periods of standing or weight bearing, physical activity, or after getting up after long periods of lethargy or sitting down. In most cases, plantar fasciitis does not require surgery or invasive procedures to stop pain and reverse damage. Conservative treatments are usually all that is required. However, every person's body responds to plantar fasciitis treatment differently and recovery times may vary.
Causes
Currently no single factor has been reliably identified as contributing to the development of plantar fasciitis. The two risk factors with the most support from current research. Decreased ankle dorsiflexion. Increased Body Mass Index (BMI) in non-athletic populations. These factors are related in that both lead to increased strain on the arch, both lead to increased compression on the heel. When dorsiflexion range of motion (ankle flexibility) is lacking, the body compensates by increasing movement of the arch. In this way, decreased ankle dorsiflexion influences pronation and places strain on the underside of the foot. Similarly, having a high BMI causes strain because it places a load on the foot that may be in excess of what the foot can support. As mentioned earlier, overpronation is thought to be a contributing factor, but studies on this have so far produced mixed results. The second way these factors relate to each other is in the way people stand. A lack of ankle flexibility and a high BMI can both cause increased pressure on the heel in standing. Keeping weight on the heels causes compression under the heel. But it also means the muscles and ligaments in the arch are not being used to balance your body weight. Lack of use, I suspect, is a greater danger than overuse. Looking beyond these potential contributors to heel pain though, there is one major factor that overshadows them all-the way footwear alters the normal function of the foot.
Symptoms
Plantar fasciitis commonly causes a stabbing pain in the heel of the foot, which is worse during the first few steps of the day after awakening. As you continue to walk on the affected foot, the pain gradually lessens. Usually, only one foot is affected, but it can occur in both feet simultaneously.
Diagnosis
Most cases of plantar fasciitis are diagnosed by a health care provider who listens carefully to your description of symptoms. During an examination of your feet, your health care provider will have to press on the bottom of your feet, the area most likely to be painful in plantar fasciitis. Because the pain of plantar fasciitis has unique characteristics, pain upon rising, improvement after walking for several minutes, pain produced by pressure applied in a specific location on your foot but not with pressure in other areas, your health care provider will probably feel comfortable making the diagnosis based on your symptoms and a physical examination. Your health care provider may suggest that you have an X-ray of your foot to verify that there is no stress fracture causing your pain.
Non Surgical Treatment
To alleviate the stress and pain on the fascia, the person can take shorter steps and avoid walking barefoot. Activities that involve foot impact, such as jogging, should be avoided. The most effective treatments include the use of in-shoe heel and arch cushioning with calf-stretching exercises and night splints that stretch the calf and plantar fascia while the patient sleeps. Prefabricated or custom-made foot orthotics may also alleviate fascial tension and symptoms. Other treatments may include activity modifications, NSAIDs, weight loss in obese patients, cold and ice massage therapy, and occasional corticosteroid injections. However, because corticosteroid injections can predispose to plantar fasciosis, many clinicians limit these injections. For recalcitrant cases, physical therapy, oral corticosteroids, and cast immobilization should be used before surgical intervention is considered. A newer form of treatment for recalcitrant types of plantar fasciosis is extracorporeal pulse activation therapy (EPAT), in which low-frequency pulse waves are delivered locally using a handheld applicator. The pulsed pressure wave is a safe, noninvasive technique that stimulates metabolism and enhances blood circulation, which helps regenerate damaged tissue and accelerate healing. EPAT is being used at major medical centers.

Surgical Treatment
Most studies indicate that 95% of those afflicted with plantar fasciitis are able to relieve their heel pain with nonsurgical treatments. If you are one of the few people whose symptoms don't improve with other treatments, your doctor may recommend plantar fascia release surgery. Plantar fascia release involves cutting part of the plantar fascia ligament in order to release the tension and relieve the inflammation of the ligament. Overall, the success rate of surgical release is 70 to 90 percent in patients with plantar fasciitis. While the success rate is very high following surgery, one should be aware that there is often a prolonged postoperative period of discomfort similar to the discomfort experienced prior to surgery. This pain usually will abate within 2-3 months. One should always be sure to understand all the risks associated with any surgery they are considering.